If you click “Continue” below, you will leave the current site and be taken to a site maintained by a third party that is solely responsible for its content. Amgen provides this link as a service to website visitors. Amgen is not responsible for the privacy policy of any third-party websites. We encourage you to read the privacy policy of every website you visit.



Identifying each patient’s risk status helps you tailor your treatment
plan to
achieve their recommended level of LDL-C.2
2018 AHA/ACC/Multi-society guideline definition of
very high risk ASCVD2


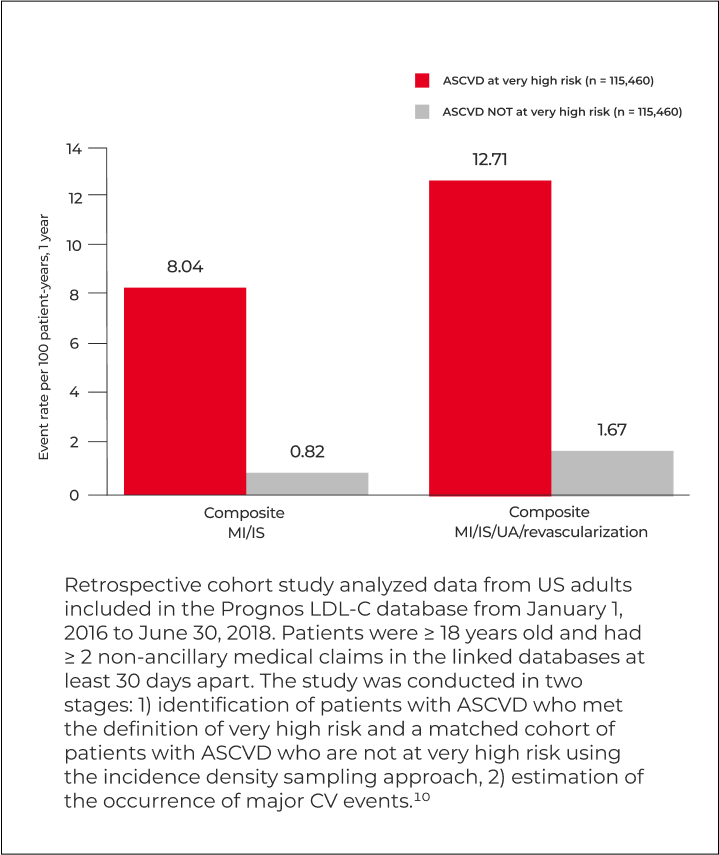
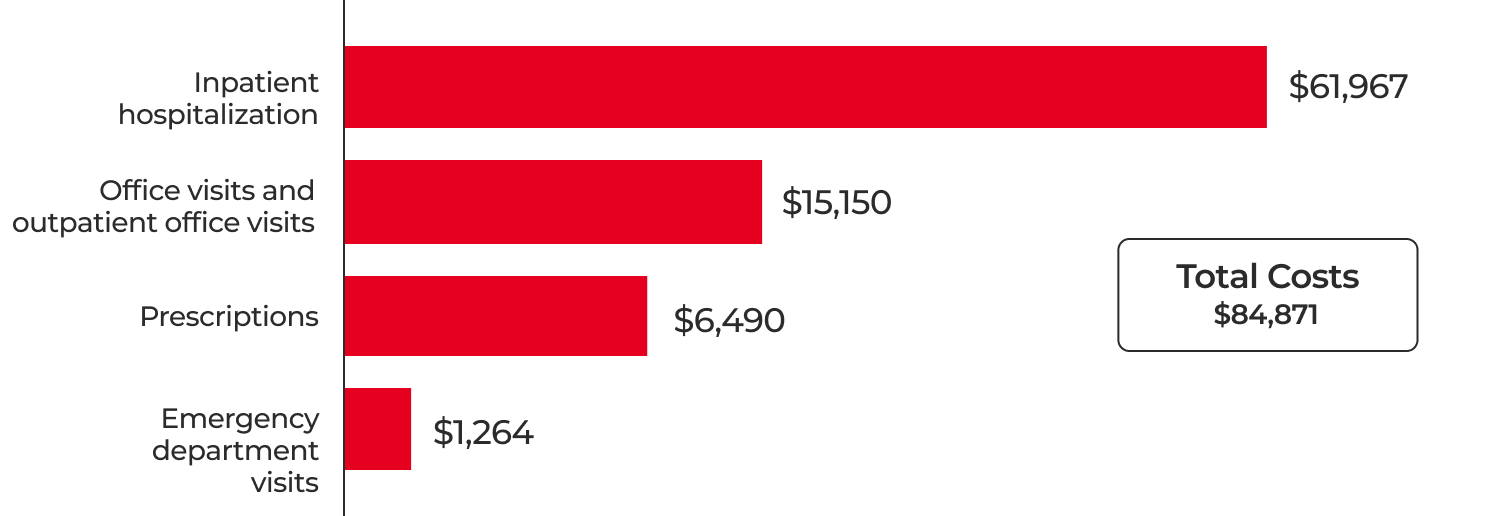
†Based on a retrospective cohort study of 16,344 patients aged 19 years or older with a history of major ASCVD event using data from the MarketScan database. This included 7,572 patients with MI (other than recent ACS), 3,551 patients with ischemic stroke, and 5,919 patients with symptomatic PAD as their history of a major ASCVD event. Patients were followed from January 1, 2016 through December 31, 2017, for recurrent ASCVD events. Very high risk was defined according to the 2018 AHA/ACC/Multi-society guidelines. Major ASCVD events included recent ACS, history of MI other than a recent ACS, history of ischemic stroke, and symptomatic PAD.10
Despite treatment with a high-intensity statin ± ezetimibe, most secondary prevention patients at very high risk have an LDL-C at or above 55 mg/dL.11,‡
‡Data included patients diagnosed with ASCVD between August 2018 to August 2023. This consisted of over 16 million patients with very high risk (VHR) ASCVD. 626,193 VHR ASCVD patients had an ASCVD event between August 2018 and August 2022 and valid LDL-C value within 12 months following most recent event. Measures on treatment based on LDL-C levels included patients with an ASCVD event between November 2018 and May 2023. Those identified as treated did not receive any additional nonstatin LLTs other than ezetimibe. The patient’s prescription activity and LDL-C levels were monitored for 3 months prior to and 3 months following their most recent event, respectively. Very high risk was defined in alignment with the 2018 AHA/ACC/Multi-society guidelines; however, persistently elevated LDL-C ≥ 100 mg/dL was not included due to data availability.11
Based on the 2022 ACC ECDP recommendation for patients with ASCVD at very high risk9
§After evaluating the optimization of lifestyle, adherence to guideline-recommended statin therapy, risk-factor control, statin-associated side effects, and escalating to high-intensity statin if not already taken.
AHA/ACC = American Heart Association/American College of Cardiology; ASCVD = atherosclerotic cardiovascular disease; ECDP = Expert Consensus Decision Pathway; MI = myocardial infarction; PAD = peripheral artery disease.
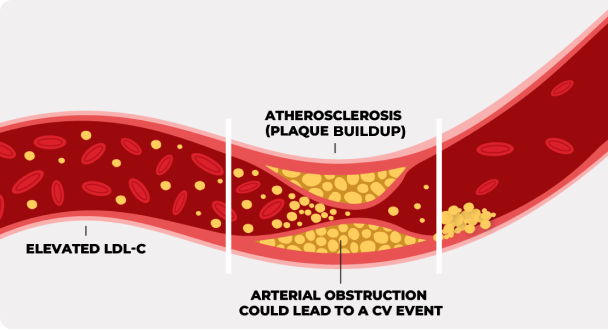
High LDL-C (bad cholesterol) can lead to serious cardiovascular events, like heart attack or stroke, especially if you have cardiovascular disease. Know more about your risk by getting your cholesterol tested. Learn how to