If you click “Continue” below, you will leave the current site and be taken to a site maintained by a third party that is solely responsible for its content. Amgen provides this link as a service to website visitors. Amgen is not responsible for the privacy policy of any third-party websites. We encourage you to read the privacy policy of every website you visit.
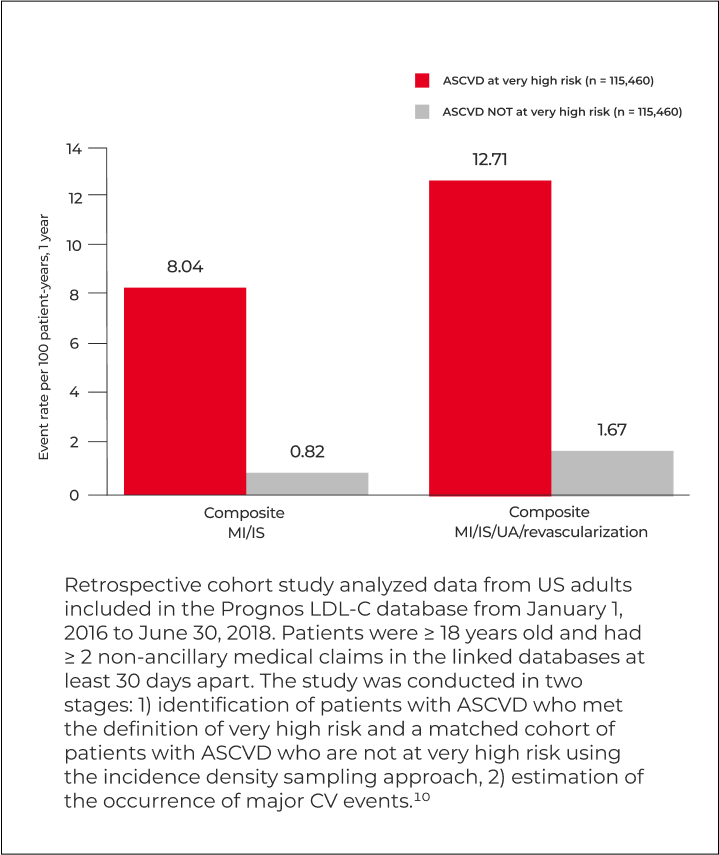
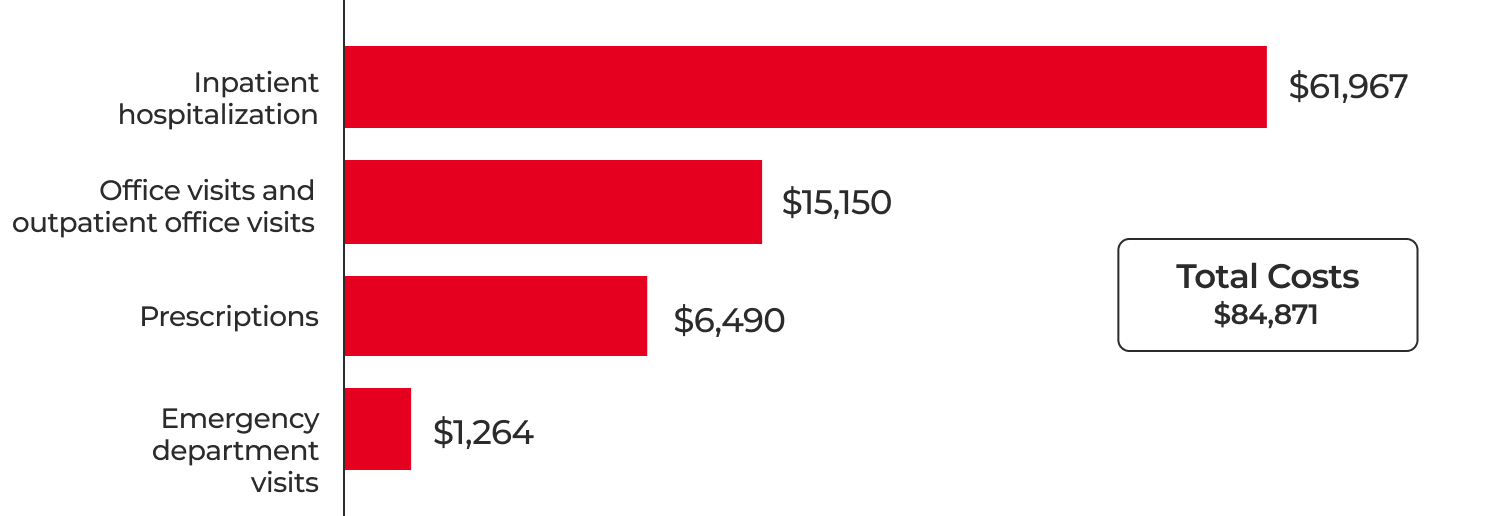
Patients with ASCVD, such as those with a recent history of myocardial infarction, experienced significantly higher rates of recurrent CV events than patients with stable atherosclerosis and no prior ischemic events. Reducing recurrent events in high-risk patients can help address the resulting economic burden to the healthcare system.1
Recurrent CV events result in significant economic burden3,4
Healthcare resource utilization and costs at 2-year follow-up for patients with a history of a CV event3,4,*
79% of patients (n = 7024) of patients who had a prior CV event
experienced another CV event requiring hospitalization
(5.8 days average stay, $41,252 average cost)3,4
Retrospective observational study based on used administrative claims from the HealthCore Integrated Research Database (HIRD). The HIRD contains longitudinal medical and pharmacy claims data for approximately 33 million members from 14 commercial health plans across the US. The study included patients aged 18 to 64 years with a diagnosis of hyperlipidemia or use of lipid-modifying medications from January 1, 2007, to December 31, 2008.
* Patients with a history of a CV event, including MI, stroke, UA, CABG, or PCI.
Watch an expert panel describe how the 2022 ACC ECDP recommendations have further evolved treatment considerations for patients with ASCVD at very high risk and their thoughts about how to implement these recommendations at a health system level to reduce CV risk and improve population health outcomes for ASCVD patients.
Below are videos from Tyler Gluckman and panelists Seth Martin, Nihar Desai, and Alan Brown, who represent Providence Heart Institute, Johns Hopkins University, Yale, and Lutheran General Hospital/Loyola University.
Resources to learn more about LDL-C management and CV event risk for ASCVD patients:
Educate health system staff about electronic health record (EHR) capabilities that can be used to identify, evaluate, and engage patients with ASCVD who are at very high risk. Health systems’ quality managers, population health managers, and clinicians can serve as champions to advocate for implementation of these capabilities. These resources provide information and tips to clinical champions to implement EHR opportunities to help meet their aims.
Support health systems in utilizing the EPIC EHR system with automated methods to help identify, evaluate, and engage patients with ASCVD at very high risk who’ve had a recent myocardial infarction. EHR systems can help address gaps in care and get patients treated according to AHA/ACC blood cholesterol management guidelines.
Support health systems in utilizing the Cerner EHR system with automated methods to help identify, evaluate, and engage patients with ASCVD at very high risk who’ve had a recent myocardial infarction. EHR systems can help address gaps in care and get patients treated according to AHA/ACC blood cholesterol management guidelines.
Support health systems in considering options for using EHR capabilities (Smart Sets, SmartTools, Flowsheets, and Discharges Summaries) to support documentation and treatment of patients with ASCVD.
Support health systems in considering options for using EHR capabilities (Smart Sets, SmartTools, Flowsheets, and Discharges Summaries) to support documentation and treatment of patients with ASCVD.
Support health systems and clinical decision makers in utilizing the Cerner and EPIC EHR systems for gathering criteria to help identify patients with ASCVD at very high risk who have had a recent myocardial infarction, outlining the criteria that clinical decision makers can utilize to define and employ for patient reports, set health maintenance reminders, and send appropriate patient follow-ups.
EHR alerts, championed in trials like PROMPT-Lipid, have shown effectiveness in enhancing guideline adherence for conditions like heart failure and cardiovascular disease. These alerts prompt physicians at the point of care, significantly increasing the likelihood of prescribing evidence-based therapies and thereby bridging the gap between clinical evidence and practice in healthcare.
ASCVD = atherosclerotic cardiovascular disease; CABG = coronary artery bypass graft; MI = myocardial infarction; PCI = percutaneous coronary intervention; UA = unstable angina.
ACC = American College of Cardiology; ASCVD = atherosclerotic cardiovascular disease; ECDP = expert consensus decision pathway.
AHA/ACC = American Heart Association/American College of Cardiology; ASCVD = atherosclerotic cardiovascular disease.