If you click “Continue” below, you will leave the current site and be taken to a site maintained by a third party that is solely responsible for its content. Amgen provides this link as a service to website visitors. Amgen is not responsible for the privacy policy of any third-party websites. We encourage you to read the privacy policy of every website you visit.
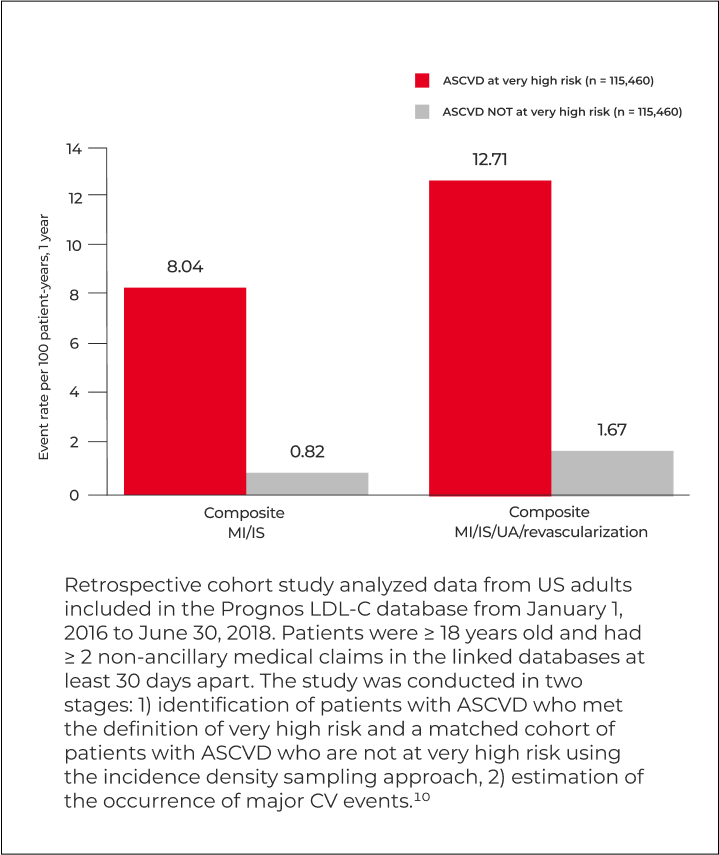
Cholesterol guidelines have consistently lowered their recommended level of LDL-C over time in recognition of the clinical benefit to reduce the risk of CV events for patients with ASCVD.1-3
The 2022 ACC ECDP currently recommends treating secondary prevention ASCVD patients at very high risk to LDL-C < 55 mg/dL and/or ≥ 50% reduction from baseline.4
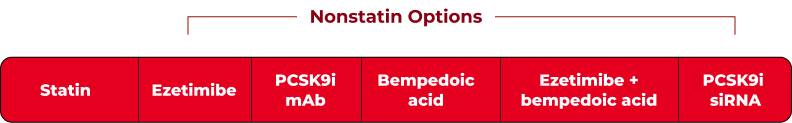
If your PATIENTS WITH ASCVD AT VERY HIGH RISK HAVE LDL-C THAT IS too high with statins alone, the 2022 ACC ECDP recommends:4
*After evaluating the optimization of lifestyle, adherence to guideline-recommended statin therapy, risk-factor control, statin-associated side effects, and escalating to high-intensity statin if not already taken.
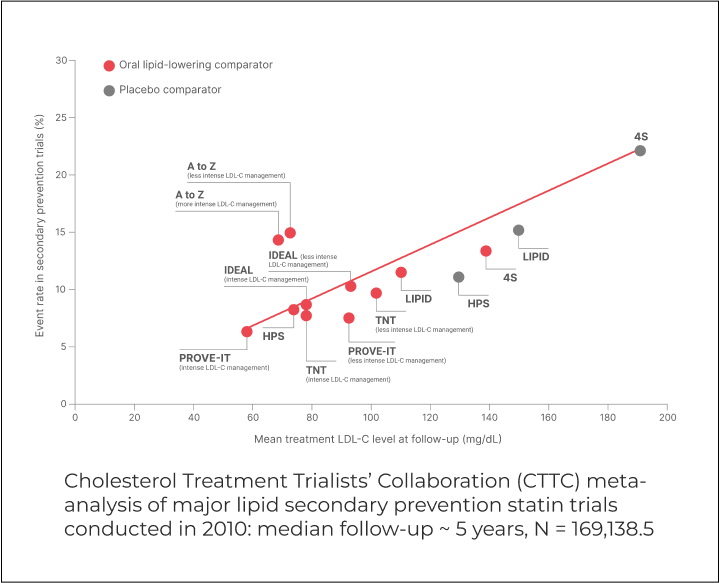
Landmark statin trials demonstrated that even patients who achieve LDL-C of 62-81 mg/dL remain at risk for future CV events. Adding nonstatin therapy may be required to address your patients’ treatment needs.
†Mean or median LDL-C after treatment.
Despite treatment with a high-intensity statin ± ezetimibe, most secondary prevention patients at very high risk have an LDL-C at or above 55 mg/dL.16,†

ACC = American College of Cardiology; ASCVD = atherosclerotic cardiovascular disease; ECDP = expert consensus decision pathway;
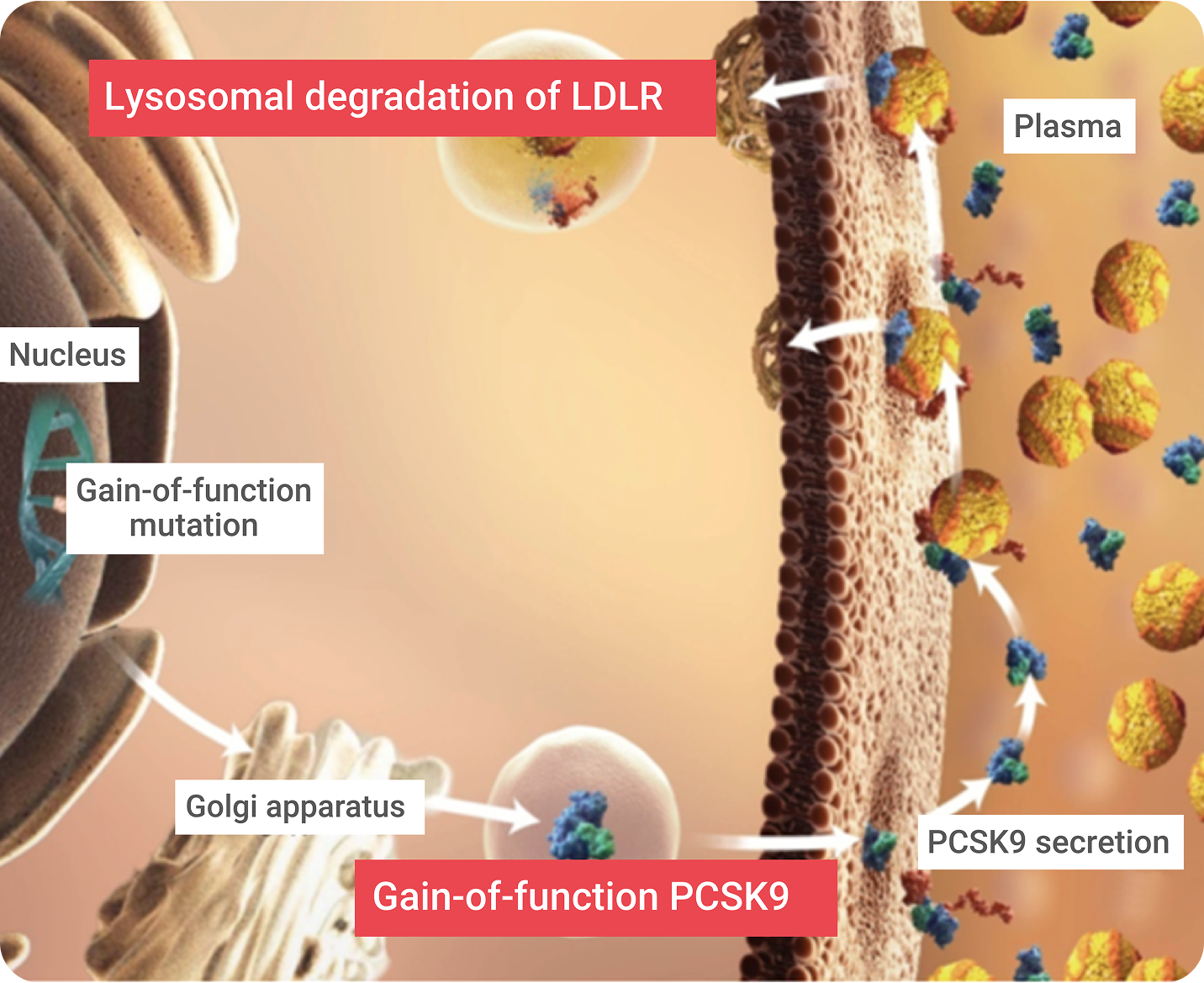
mAb = monoclonal antibody.